Skin Cancer
The skin is the largest organ in our body, and is made up of two major layers (epidermis and dermis), as well as various types of cells. The top (or outer) layer of the skin, the epidermis, is composed of three types of cells: flat, scaly cells on the surface called squamous cells; round cells called basal cells; and melanocytes, cells that provide skin its color and protect against skin damage.
The inner layer of the skin, the dermis, is the layer that contains the nerves, blood vessels, and sweat glands. Skin cancer is a disease in which cancerous (malignant) cells are found in the outer layers of your skin.
What Are the Symptoms of Skin Cancer?
Most skin cancers can be cured if diagnosed and treated early. Aside from protecting your skin from sun damage, it is important to recognize the early signs of skin cancer.
The ABCDEs of melanoma are a helpful guide: (A) Asymmetry; (B) Borders; (C) Color; (D) Diameter; (E) Evolution. The symptoms of melanoma skin cancer include:
- Moles that are different on one side (asymmetry)
- Irregular borders of a mole
- Color variation including shades of brown and black, which could be concerning
- Diameter or the size—if the mole is larger than 6 mm, a doctor should evaluate it
- Moles or lesions that are different than the rest, or change in size, shape, or color over time are concerning (evolution)
Symptoms of non-melanoma skin cancer include:
- Itchy patches of skin that may crust over or are very painful
- Bumps or skin spots that bleed easily or crust over frequently
- Nodules (aggregation or swelling or abnormal swelling) that do not go away. These may be clear, a pearl-like color, or even red, pink, or white.
- Skin sores that do not heal
- A scar-like bump that was not caused by injury or trauma
If you notice any of the factors listed above, see your primary care provider, or an ENT (ear, nose, and throat) specialist, or otolaryngologist, right away. If you have a spot or lump on your skin, your ENT specialist may remove the growth and examine the tissue under the microscope. This is called a biopsy. A biopsy can usually be done in the ENT specialist’s office, and usually involves numbing the skin with a local anesthetic. Examination of the biopsy under the microscope will tell the doctor if the skin lesion is a cancer (malignancy).
What Causes Skin Cancer?
Most skin cancers occur on sun-exposed areas of skin, and there is a lot of scientific evidence to support ultraviolet (UV) radiation as a causative factor in most types of skin cancer. Family history is also important, particularly in melanoma. The lighter your skin type, the more susceptible you are to UV damage and to skin cancer. You have a higher risk of developing skin cancer, and should be particularly careful about sun exposure, if you have any of these factors:
- Long-term sun exposure
- Fair skin (typically blonde or red hair with freckles) and lighter eye color
- Place of residence (increased risk in southern climates)
- Presence of moles, particularly if there are irregular edges, uneven coloring, or an increase in the size of the mole
- Family history of skin cancer, particularly melanoma
- Use of indoor tanning devices
- Severe sunburns as a child
- Non-healing ulcers or nodules in the skin
- History of organ transplant or other immune system suppression
What Are the Different Types of Skin Cancer?
There are several types of cancer that originate in the skin. The most common types are basal cell carcinoma and squamous cell carcinoma. These types are classified as non-melanoma skin cancer. Melanoma is the third type of skin cancer. It is less common than basal cell or squamous cell cancers, but potentially much more serious. Other types of skin cancer are rare.
Basal cell carcinoma is the most common type of skin cancer (70 percent of all skin cancers). It typically appears as a small raised bump that has a pearly appearance. It is most commonly seen on areas of the skin that have received excessive sun exposure. These cancers may spread to the skin surrounding them, but rarely spread to other parts of the body.
Squamous cell carcinoma (20 percent of all skin cancers) is also seen on the areas of the body that have been exposed to excessive sun (nose, lower lip, hands, and forehead). Often this cancer appears as a firm red bump or ulceration of the skin that does not heal. Squamous cell carcinomas can spread to lymph nodes in the area.
Melanoma is a skin cancer (malignancy) that arises from the melanocytes in the skin. This makes up five percent of skin cancers. Melanocytes are the cells that give color to our skin. These cancers typically arise as pigmented (colored) lesions in the skin with an irregular shape, irregular border, and multiple colors. It is the most harmful of all the skin cancers, because it can spread to lymph nodes or other sites in the body. Fortunately, most melanomas have a very high cure rate when identified and treated early.
What Are the Treatment Options?
There are varieties of treatments available to treat skin cancer, including surgery, radiation therapy, and chemotherapy. Treatment for skin cancer depends on the type and size of cancer, your age, and your overall health.
Surgery is the most common form of treatment. It generally consists of an office or outpatient procedure to remove the lesion and check the edges, or margins, to make sure all the cancer was removed. For basal cell and squamous cell carcinomas, excision is frequently done using a specific technique called Mohs surgery, which gives the best chance to include all margins, while still minimizing the size of the defect. The site may then be repaired with simple stitches or skin from the same area or a different area of your body.
For melanoma treatment, your ENT specialist might also recommend doing a biopsy of the lymph node with the highest chance of having tiny microscopic metastatic cancer cells called a sentinel lymph node biopsy. If this biopsy is positive, further removal of more lymph nodes might be needed.
Sometimes radiation may be used as definitive therapy or additional treatment after surgery. For non-melanoma skin cancers, chemotherapy is not used as primary therapy, and its use after surgery is controversial. For melanomas, chemotherapy and medications that modulate the immune system may be used in more advanced cases.
What Questions Should I Ask My Doctor?
- What are my risk factors for developing skin cancer and what can I do to minimize this risk?
- What symptoms should I be looking for to see if I have skin cancer?
- What type of skin cancer do I have?
- What are the treatment options for my skin cancer?
- What stage is my skin cancer?
- Are there any topical medications that can be used to treat the skin cancer?
- If surgery is indicated, what kind of surgery will I need? Can it be done in the office or will it require general anesthesia?
- What kind of reconstruction (repair of the wound) will I need if I have surgery?
- What will the scar look like?
- Is there a chance for the cancer to have spread to another part of my body and do I need any imaging (such as a CT scan) to evaluate?
- What is my risk of having other skin cancers?
- What kind of follow up do I need after treatment of my skin cancer?
- Are there any side effects of the treatment?
- What happens if the cancer comes back or spreads?
- What should I be looking out for to see if the cancer may be coming back?
- Are there any clinical trials that may apply to me?
Sinusitis
Have you ever felt like you had a cold that wouldn’t go away? If symptoms of discolored nasal drainage and blockage hang around for more than 10 days, or worsen after they start getting better, there’s a good chance you have sinusitis, an infection or inflammation of the sinuses.
Sinuses are hollow spaces in the bones around the nose that connect to the nose through small, narrow channels. Sinusitis, also called rhinosinusitis because the symptoms involve both the nose and the sinuses, affects about one in eight adults annually. For many, the inflammation starts when viruses or bacteria infect your sinuses (often during a cold), and begin to multiply. Part of the body’s reaction to the infection causes the sinus lining to swell, blocking the channels that drain the sinuses. This causes mucus and pus to fill up the nose and sinus cavities. For others, the symptoms and inflammation may be the result of the nose and sinuses reacting to other things in the environment, but not be an infection.
Acute vs. Chronic Sinusitis
Because sinusitis simply means inflammation of the sinuses, the word alone includes a variety of similar problems. Acute sinusitis is when the symptoms occur for less than four weeks. A diagnosis of chronic sinusitis requires that the symptoms last longer than 12 weeks. Sometimes these are caused by the same thing, but often chronic and acute sinusitis are very different from each other. Your primary care provider or an ENT (ear, nose, and throat) specialist, or otolaryngologist, can help sort out what type of sinusitis you have and how to treat it. Recurrent acute sinusitis is when someone has four or more sinus infections (acute sinusitis) in one year but does not have symptoms in between those infections.
What Are the Symptoms of Sinusitis?
You have acute sinusitis when you have had cloudy or colored drainage from your nose for up to four weeks, plus one or more of the following symptoms:
- Stuffy, congested, or blocked nose
- Pain, pressure, or fullness in the face, head, or around the eyes
- Long-lasting cold symptoms
- Symptoms that do not improve within 10 days of getting sick, or initially get better then worsen again
You might have chronic sinusitis if you have at least two of the four symptoms note below for at least 12 weeks. An ENT specialist would also need to see polyps, pus, or thickened mucous in nose, or get a CT scan, to fully diagnose chronic sinusitis. Possible symptoms include:
- Stuff congested, or blocked nose
- Pain, pressure or fullness in the face, head or around the eyes
- Thickened nasal drainage
- Loss of smell
What Causes Sinusitis?
Viruses or bacteria usually cause acute sinusitis. Acute viral sinusitis is likely if you have been sick for less than 10 days and are not getting worse. Acute bacterial sinusitis is when you do not improve at all within 10 days of getting sick, or when you get worse within 10 days after beginning to get better.
Chronic sinusitis, however, is usually caused by prolonged inflammation, instead of a long infection. Infection can be a part of chronic sinusitis, especially when it worsens from time to time, but is not usually the main cause. The exact cause cannot always be determined; for some reason the nose and sinuses are overreacting to what they think is an infection.
Are There Any Related Conditions or Complications?
Migraine headaches or tension headaches can cause symptoms of sinus pain or pressure. If you have sinus headaches without discolored drainage, talk to your primary care provider, or an ENT specialist, about the possibility of migraine headaches causing sinus pain or pressure and medications options for migraine treatment. Sometimes inflammation of the nasal cavity can also cause drainage and nasal congestion, but not involve your sinuses.
What Are the Treatment Options?
Sinusitis is treated differently based on the cause. Most cases of acute sinusitis, about 98 percent, are caused by a virus, not bacteria, and should not be treated with antibiotics. Acute viral sinusitis may be treated using pain relievers such as acetaminophen or ibuprofen, steroid nasal sprays, or salt water irrigation in the nose. These treatments are also good options for acute bacterial sinusitis. Most people get better naturally from acute bacterial sinusitis, called “watchful waiting,” but some patients with acute bacterial sinusitis may get better faster with an antibiotic.
Chronic sinusitis is treated differently than acute sinusitis. Because chronic sinusitis is caused more by inflammation than infection, the treatments for chronic sinusitis aim to control the inflammation. Salt water nasal irrigation and/or nasal steroid sprays are the main treatments for the symptoms of chronic sinusitis. Antibiotics may sometimes be helpful but not always.
Other factors, including allergies, nasal polyps, asthma, and problems with the body’s ability to fight infections, can go along with sinusitis and make it worse unless they are also treated.
X-rays or CT scans of the sinuses are not necessary to diagnose uncomplicated sinusitis if you have the symptoms of sinusitis (discharge plus pressure or blockage). If your doctor suspects a complication or if you have repeated episodes or prolonged sinus symptoms, a CT scan of your sinuses may be needed.
Surgery
Surgery is not recommended for acute sinusitis except in rare circumstances. Sometimes the sinus infection can spread to the eye, face, or brain; this would be considered an emergency, and surgery may be needed to reverse the infection and keep it from spreading.
For chronic sinusitis, surgery is an option when the symptoms cannot be controlled with medications and other treatments. The most common type of surgery for the sinuses is called endoscopic sinus surgery; a pencil-sized scope (endoscope) is used to see inside the nose and sinuses and guide the surgery. The surgery widens the natural drainage pathways between the sinuses and the nose, allowing mucus to get out of the sinuses and air to get in. Medications that are delivered into the nose and sinuses, like sprays and irrigations, can also get into the sinuses better after surgery.
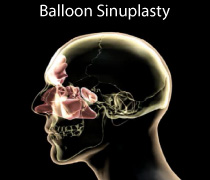
Balloon sinus ostial dilation (BSOD) is a newer treatment option where an endoscope is also used, but instead of carefully removing the bone and tissue that may be blocking a sinus, a balloon is used to make the sinus openings bigger. Balloon dilation may not be appropriate for every type of chronic sinusitis and cannot be used on all of your sinuses, but can be helpful depending on your circumstances.
What Questions Should I Ask My Doctor?
- Do I have a bacterial infection?
- Do I need to take antibiotics if I have acute bacterial sinusitis?
- Should I get an X-ray or CT scan of my sinuses when I have sinusitis?
- What else could be causing my symptoms?
References
Diagnosis of acute sinusitis: http://www.entnet.org/sites/default/files/uploads/PracticeManagement/Resources/_files/adult-sinusitis-patient-info-diagnosis-of-sinusitis.pdf
Treatment of acute bacterial rhinosinusitis: http://www.entnet.org/sites/default/files/uploads/PracticeManagement/Resources/_files/adult-sinusitis-patient-info-treating-acute-bacterial-rhinosinusitis.pdf
Clinical Practice Guidelines for Adult Sinusitis: http://journals.sagepub.com/doi/full/10.1177/0194599815572097
Sinus Headaches
Not every headache is the result of sinus and nasal passage problems. For example, many patients visit an ENT (ear, nose, and throat) specialist, or otolaryngologist, to seek treatment for what they think is a sinus headache, only to learn they actually have a migraine or tension headache. The confusion is common, as a migraine can cause irritation of the “trigeminal,” or fifth cranial nerve, a nerve with branches in the forehead, cheeks, and jaw. This may produce pain and nasal symptoms in or near the sinus cavity.
Pain in the sinus area does not automatically mean that you have a sinus disorder. Sinus headache is a common term used by patients and some healthcare providers to describe pain or pressure in the face, over the cheeks or forehead, or between or behind the eyes (where the sinuses are located). Sinus headache, however, is not a medical diagnosis, but rather a description of symptoms of headaches.
What Are the Symptoms of Sinus Headaches?
Patients with migraines or tension headaches commonly have sinus and nasal symptoms during their headaches, including sinus pressure, sinus pain, nasal congestion or runny nose. Studies of patients who have self-diagnosed or been diagnosed with sinus headaches were found to have migraines or tension headaches in more than 80 percent of cases; only three to five percent of these patients had sinusitis.
Symptoms of sinusitis and migraine headaches can be similar, which can be confusing about what is causing sinus pain and pressure. Migraines and headaches can cause the following nasal symptoms:
- Pain and pressure around the eyes, across the cheeks, and the forehead
- Nasal congestion
- Runny nose
- Eye redness, tearing, or eyelid swelling
- Symptoms on one or both sides of the face
Sinusitis is associated with nasal congestion or obstruction and a thick nasal discharge, sometimes with facial pain, pressure, or a feeling of fullness. However, facial pain or pressure or fullness without cloudy or colored nasal discharge is most likely not a sinus infection.
How Do You Diagnose Sinus Headaches Caused by Migraines?
Sinus headaches are most likely due to migraines or tension headaches. Migraines are diagnosed by symptoms, including the frequency and severity of symptoms, family history, and by physical exam. Migraines can also include nausea and vomiting. These episodes may be triggered by hormonal changes, lack of sleep, certain foods or alcohol or caffeine, stress, or environmental changes like weather, altitude changes, or allergens. Many patients with migraines have family members who also experience migraine headaches.
If you have unusual or severe symptoms, additional tests such as an MRI of the brain may be ordered to rule out more serious conditions that can cause headache pain, such as tumors or bleeding around the brain. If you have repeated episodes of sinus pain and pressure, a nasal endoscopy (a pencil-sized scope used to see inside the nose and sinuses) or imaging such as an MRI or CT scan can determine if sinus pain or pressure is due to a sinus infection or other sinus pathology. A normal sinus CT scan while you have symptoms could help rule out sinusitis, and determine if migraines, headaches, or other causes of facial pain and pressure are causing the sinus symptoms.
Other causes of facial pain and pressure can include temporomandibular joint (TMJ) syndrome, clenching or grinding your teeth, trigeminal nerve pain, temporal arteritis (associated with scalp pain, pain in the temple, jaw pain, and vision changes on one side), dental infection, or other neurologic causes of facial pain.
What Are the Treatment Options?
Your primary care provider, or a neurologist, can provide recommendations for treating your headaches based on their severity and frequency, and can rule out more serious causes of your headache. Treatment for migraines includes both over-the-counter and prescription medications (also known as acute or abortive therapies) and preventative medications for patients with severe or frequent headaches, or if headaches are present for more than 15 days per month.
Over-the-counter pain medications such as ibuprofen or acetaminophen can also be associated with rebound headaches or medication-overuse headaches if taken too often. Tell your doctor how often you take pain medications for headaches. Avoid triggers, and talk to your doctor about your sleep habits. Keep a headache diary to record your headache symptoms, triggers, and treatments.
Sinus headaches caused by migraines or tension headaches should not be treated with antibiotics. Because there are similar symptoms between acute sinusitis and migraine headaches with nasal and sinus symptoms, it can be difficult to tell if your symptoms are truly a sinus infection. Sinus pain and pressure without discolored nasal discharge is most likely not a sinus infection. If you have been diagnosed with frequent sinus infections and have been treated with repeated episodes of antibiotics without improvement, migraines or tension headaches could be causing your sinus pain and pressure.
What Questions Should I Ask My Doctor?
- I get frequent sinus headaches. Is this the same thing as having a migraine or tension headache?
- If I also have trouble breathing and have a heavy discharge from my nose, what does that mean?
- Are migraines a symptom of a potentially bigger problem? Should I get an MRI or see a neurologist?
- I’ve tried over-the-counter pain medications like ibuprofen and acetaminophen, but they don’t always work. Are there other prescription medications I could use instead?
Sialadenitis
Sialadenitis is inflammation and enlargement of one or more of the salivary (spit) glands. The salivary glands are responsible for producing and storing saliva. The three major salivary glands are the “parotid” (on the sides of the face in front of the ears), “submandibular” (under the jaw), and “sublingual” glands (under the tongue). All of these glands empty saliva into the mouth through small tubes called ducts.
Sialadenitis can occur due to infection, salivary stones, or an underlying autoimmune disorder. It usually affects the parotid and submandibular glands and is most common among the elderly.
What Are the Symptoms of Sialadenitis?
The symptoms of sialadenitis can include:
- Swelling in the cheek and neck region, especially after eating
- Mouth or facial pain
- Dry mouth
- Foul taste or gritty feeling in the mouth
- Fever
- Chills
- Redness over the side of the face or upper neck
- Pus in the mouth
What Causes Sialadenitis?
Sialadenitis can be caused by a viral infection (such as mumps), bacterial infection, or an autoimmune disease such as Sjogren’s syndrome (see below). Bacterial infections can happen when the flow of saliva is blocked due to stones in the salivary duct or a narrowing of the duct. Dehydration can also cause bacterial infections by reducing saliva flow. Recent illness and the use of antihistamines, beta-blockers, or diuretics can lead to dehydration. Radioactive iodine (RAI), sometimes used for treatment after surgery of thyroid cancer, can also result in salivary gland scarring and sialadenitis because some of the radioactivity can be accumulated in the salivary glands.
Sjogren’s syndrome is an autoimmune disease which effects salivary glands and the “lacrimal” glands of the eyes. This chronic inflammatory disorder causes decreased saliva production in the mouth and decreased tear production in the eyes. In addition to dry mouth and eyes, there may be symptoms of fatigue, muscle aches, or rashes. In extreme cases, Sjogren’s syndrome may affect the lungs, kidneys, liver, and nervous system. People with Sjogren’s syndrome may also have swelling of the parotid or submandibular glands, as well as an unexplained increase in dental cavities or tooth decay.
An ENT (ear, nose, and throat) specialist, or otolaryngologist, may diagnose Sjogren’s syndrome based on persistent symptoms of dry eyes and/or mouth, parotid gland enlargement, and abnormal blood test results. A lip biopsy can confirm the diagnosis. Sjogren’s syndrome is treated conservatively with symptomatic relief. Oral rinses and hydration are advised along with lubricating eye drops.
What Are the Treatment Options?
Treatment for sialadenitis includes good oral hygiene, increasing fluid intake, massaging over the affected gland, applying a warm compress, and using candies or foods which increase saliva (such as lemon drops). In some cases, if the cause is bacterial, antibiotics may be prescribed. Antibiotics are not useful for viral infections. An endoscopic procedure with a very small camera (called Sialendoscopy) can be used in certain cases.
Most salivary gland infections resolve or are cured with conservative treatment after one week. In rare cases of recurrent sialadenitis, surgery may be necessary to remove part or all of the gland.
What Questions Should I Ask My Doctor?
- Is there anything I can do to decrease the chances of future episodes of sialadenitis?
- Do any of my current medications increase my risk of sialadenitis?
- How do I know if there is an underlying disease that is causing my sialadenitis?