Spasmodic Dysphonia
Spasmodic dysphonia (SD) is a voice disorder that causes involuntary spasms or contractions of the vocal cords, interrupting speech and affecting the quality of a person’s voice. The voice may sound broken, strained, or breathy depending on the type of SD. The two most common types of SD are the adductor type (ADSD), where the vocal cords close together too tightly during certain sounds, and the abductor type (ABSD), where the vocal cords spasm open during certain sounds. Although it can start at any time during life, SD seems to begin more often in middle-age. The disorder affects women more often than men. Onset is usually gradual with no obvious cause.
What Are the Symptoms of SD?
Symptoms of SD can vary from mild to severe and may include:
- Gradual or sudden difficulty speaking
- Breaks in the voice during speech
- Increased effort with speaking
- Normal voice with non-speaking tasks, for example, when singing or laughing
What Causes SD?
Although the exact cause of SD is unknown, evidence suggests that SD involves an area at the base of the brain where involuntary muscle movement is regulated and is, therefore, neurological in origin. When this nervous system regulator does not work properly and produces incorrect signals, this may cause voice muscles to contract or relax more than they should or at the wrong time.
Researchers are examining different areas of the brain that may be involved, including the basal ganglia, which helps to regulate movement; the cerebellum, which helps to control balance; and the cortex, which initiates movement and recognizes sensation. There may also be a genetic relationship as genes have been identified in other forms of movement disorders known as dystonia.
What Are the Treatment Options?
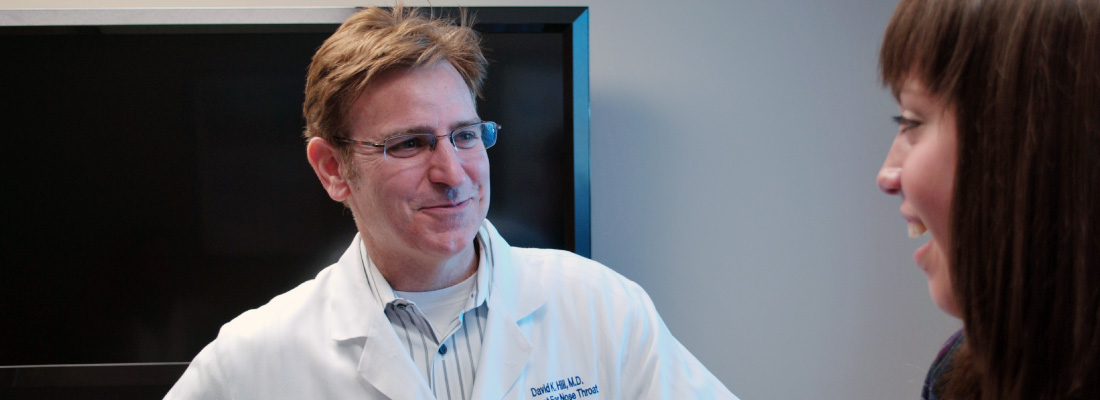
Generally, an ENT (ear, nose, and throat) specialist, or otolaryngologist, and a speech language pathologist will perform a comprehensive exam, including a review of the patient’s medical history and symptoms and a visualization of vocal fold movement using a special camera called a flexible laryngoscope through the nose. The patient may be asked to read or repeat several phrases so the physician can assess different voice qualities (i.e., overall severity, breaks, roughness, strain, breathiness). SD is diagnosed by listening to the specific voice changes during these speech tasks and distinguishing it from other types of hoarseness, in addition to examining the larynx.
There is no cure for SD. Treatments are often focused on decreasing the spasms or by improving control of the associated symptoms. Specific treatment options depend on each patient but may include:
Botulinum toxin A injections—Botulinum toxin A (Btx A) is injected into the laryngeal muscles that control the opening (abduction) and closing (adduction) of the vocal cords. Btx A blocks nerve impulses at the muscle receptor site. This weakening of the injected muscle(s) is only temporary, varies from person to person, and is based on dosage, but the average duration of the effect is three to four months. Possible side effects are usually brief and include a breathy or whispery voice, difficulty swallowing, or pain/soreness at the site of injection. Commonly, Btx A injection to the vocal cords results in a period (approximately two months) of close-to-normal voice for many ADSD patients. Btx A is the most reliable and thoroughly evaluated treatment for SD.
Voice therapy—Voice therapy cannot cure SD, but with the help of a speech language pathologist patients may be able to learn how to readjust breathing patterns, phonation, resonance, and articulation to make their voice work more efficiently and to better manage symptoms, such as breaks, strain, roughness, and breathiness. Voice therapy should incorporate individual goals, such as strategies for speaking in groups, speaking on the phone, speaking with less effort, and managing quality of life issues associated with SD.
Surgical options—Several surgical options have been used to try to treat SD, yet surgery for SD remains a controversial topic. Most procedures are designed to treat ADSD. In Type II Thyroplasty surgery, the surgeon separates the vocal cords slightly to reduce the severity of spasms, which can result in a weaker or breathier voice. Another procedure, called Selective Laryngeal Adductor Denervation-Reinnervation (SLAD-R), involves cutting the nerves to the vocal cord muscles and reinnervating those muscles with a different nerve. Long-term studies have not been published on the results of these surgeries for SD.
What Questions Should I Ask My Doctor?
- What caused my spasmodic dysphonia?
- How is spasmodic dysphonia diagnosed?
- Is spasmodic dysphonia genetic?
- Will I have this for the rest of my life? Will my voice get worse with time?
- Can I retrain my voice to sound like it used to sound?
- What are the best treatment options for me and my form of SD?
- Is BOTOX® an option for me, and what are the possible side effects? How long and how often will I need additional injections?
Note: This article was prepared in coordination with the National Spasmodic Dysphonia Association.
Salivary Gland Disorders
The salivary glands are found in and near your mouth, face, and neck. Dehydration is a risk factor for certain salivary gland disorders. To help maintain good oral health, it’s important to drink lots of liquid every day to promote good saliva production.
The major salivary glands include the parotid (on the cheek and under the ear), submandibular (under the jaw), and sublingual (under the tongue) glands. These glands produce saliva, which helps moisten the mouth, initiates food digestion, and helps protect teeth from decay. There are also many tiny, minor salivary glands located along the lips, inside the cheek, mouth, and throat.
What Are the Symptoms of Salivary Gland Disorders?
Problems with the salivary glands may produce symptoms such as:
- Blocked saliva flow
- Difficulty eating
- Swelling in the gland(s) of the cheek and neck
- Pain in the gland(s)
- Repeated infections
- Growths or lumps inside the glands or neck
What Causes Salivary Gland Disorders?
Saliva obstruction—Saliva flow can be blocked in the parotid and submandibular glands or ducts either by stones or narrowing inside the ducts. A blocked saliva duct can lead to pain and swelling of the saliva gland. Typically, the glands will swell during a meal for a few minutes before gradually subsiding, only to enlarge again at the next meal. Infection with severe pain and swelling can develop if the gland is blocked for a long time without the ability to release the built-up saliva. If persistent gland swelling is left untreated, the glands may develop a severe infection or abscess.
You may experience a swelling or enlargement of nearby lymph nodes with salivary blockage. These lymph nodes are the structures in the upper neck that often become tender during a common sore throat. In fact, some of these lymph nodes are located on or deep within the parotid gland, or near the submandibular glands. When these lymph nodes become enlarged from infection, you may have a red, painful swelling in the area.
Tumors—Cancerous (malignant) or noncancerous (benign) tumors usually show up as painless lumps or enlargements. Tumors rarely involve more than one gland and are detected as a growth in the parotid, submandibular area, on the palate, floor of mouth, cheeks, or lips. An ENT (ear, nose, and throat) specialist, or otolaryngologist, should check these enlargements.
Cancerous tumors of the major salivary glands can grow quickly, may be painful, and can cause loss of movement in part, or all, of the affected side of the face. These symptoms should also be checked immediately by an ENT specialist.
Other disorders—Enlarged or inflamed salivary glands can also be caused by autoimmune diseases, such as HIV and Sjögren’s syndrome, where the body’s immune system attacks the salivary glands. Dry mouth or dry eyes are symptoms of Sjögren’s syndrome. This may occur with other systemic diseases, such as rheumatoid arthritis. Diabetes may cause painless enlargement of the salivary glands, especially the parotid glands.
What Are the Treatment Options?
If your doctor or ENT specialist suspects a salivary gland obstruction, they may numb the opening of the salivary ducts in your mouth and dilate the duct to help an obstructive stone pass. Imaging with a CT scan or ultrasound may also reveal where the calcified stones are located.
If a mass is found in the salivary gland, it’s helpful to obtain a CT or MRI scan. Sometimes, a fine needle aspiration biopsy in the doctor’s office helps determine what’s going on. Rarely, dye will be injected through the parotid duct and an X-ray, called a sialogram, of the gland is taken. Alternatively, small endoscopes, called sialendoscopes, can be used to examine the salivary ducts and diagnose and treat an obstruction from stones or stenosis.
A lip biopsy of minor salivary glands may be needed to identify certain autoimmune diseases, such as Sjögren’s syndrome.
Treatment of salivary diseases falls into two categories—medical and surgical—and depends on the nature of the problem. If it is due to diseases or disorders that involve the whole body, not one isolated area, then the underlying problem must be treated. This may require consulting with other specialists. If the disorder relates to salivary gland obstruction and infection, your doctor or ENT specialist may prescribe antibiotics and recommend increasing your fluids.
If a mass has developed within the salivary gland, removal of the mass may be recommended. Most masses in the parotid gland area are noncancerous. When malignant masses are located within the parotid gland, it may be possible to surgically remove them while preserving most of the facial nerve within the gland that moves the face muscles, including those for the mouth and eyes. Radiation treatment is sometimes recommended after surgery. This is typically administered four to six weeks after the surgical procedure to allow adequate healing before irradiation.
The same general principles apply to masses in the submandibular area or in the minor salivary glands within the mouth and upper throat. Noncancerous masses are best treated by conservative measures or surgery. If the lump in the vicinity of a salivary gland is a lymph node that has become enlarged due to cancer from another site, your ENT specialist will recommend a different treatment plan.
What Questions Should I Ask My Doctor?
- What is the cause of my salivary gland problem?
- Do I need further evaluation with imaging or a needle biopsy?
- What are the signs of salivary gland infection? When do I need antibiotics?
- What will I experience if my salivary gland(s) needs to be removed?
- What are the possible side effects of surgery or radiation therapy?
- Can you recommend medications or other conservative treatments?
- How many times have you performed this type of procedure?
Ramsay Hunt Syndrome
Ramsay Hunt syndrome (RHS), also known as herpes zoster oticus, is a rare yet severe condition that causes facial weakness or paralysis and a rash on the outer ear. The same virus that causes chickenpox and shingles, the varicella zoster virus, can spread and affect the facial nerve, which controls movement of each side of the face. The virus also causes the ear to break out in a serious, painful rash.
What Are the Symptoms of RHS?
Symptoms of RHS all occur on the same side of the face but may not occur at the same time. They include:
- Decreased movement of one side of the face
- Painful rash with fluid-filled blisters on the ear skin and ear canal
- Hearing loss, ringing in the ear
- Vertigo
- Dry mouth, dry eyes
- Change in taste
What Causes RHS?
RHS is caused by a reactivation of the herpes zoster virus that may have caused chickenpox in childhood. This virus stays in the body and can attack the nerve that controls facial movements and the sensory nerve that supplies the face. This virus can also cause shingles, a stinging rash on one side of the body, in adults. RHS occurs in one out of every 20,000 people each year, usually in older adults but rarely in children. It can affect men and women equally.
What Are the Treatment Options?
Treatment for RHS includes antiviral therapies and corticosteroids. Starting these medications as soon as possible helps improve recovery. When symptoms are severe, these medications can be given intravenously (IV) in the hospital.
RHS can be a very painful condition, too. Pain control with multiple types of medications is important during treatment and even after the rash goes away and facial movement returns. Because patients have difficulty closing the eye due to facial nerve paralysis, eye moisturization and lubrication is very important. Medication for nausea and dizziness is also helpful during treatment to support recovery.
What Questions Should I Ask My Doctor?
- Is my facial paralysis caused by RHS or by another condition?
- Is my facial paralysis going to be permanent?
- Will my hearing loss, ringing in the ear, and/or vertigo become permanent?
- How can I protect my eye?
- Will this virus cause permanent nerve fiber pain (postherpetic neuralgia) once it goes away? How can I treat that?
Pediatric Gastroesophageal Reflux Disease (GERD)
Acid reflux occurs when acidic stomach contents flow back into the esophagus, the swallowing tube that leads from the back of the throat to the stomach. In some children, when reflux happens so frequently and is so severe that it causes complications, it is known as pediatric gastroesophageal reflux disease (GERD). An estimated five to eight percent of children have pediatric GERD. In babies, reflux is called spit up, and is normal and expected. In older children, the signs of reflux can be burping, stomach aches, and heartburn.
Complications include failure to gain weight, bleeding, breathing problems, hoarseness, and/or inflammation of the esophagus, known as esophagitis. Researchers have found that one in 10 infants younger than 12 months with GERD develop significant complications, but as infants grow their improved muscle control and the ability to sit up often resolves many instances of GERD.
What Are the Symptoms of Pediatric GERD?
GERD is common in adults, but children have a harder time describing this sensation. They may complain of stomach aches or chest discomfort, particularly after meals. Other symptoms include:
- Crying or irritability
- Poor appetite, or feeding and swallowing problems
- Weight loss or poor weight gain
- Wet burps or vomiting, or regurgitation
- Stomach aches
- Abdominal and/or chest pain
- Sore throat
- Hoarseness
- Asthma or wheezing
- Chronic coughing and throat clearing
- Chronic sinusitis
- Ear infections and/or fluid in the ear
- Tooth decay
What Causes Pediatric GERD?
GERD occurs when a valve at the lower end of the esophagus doesn’t work properly. Normally, this muscle closes to keep acid in the stomach and out of the esophagus. During the first year, infants frequently spit up. This is called laryngopharyngeal reflux (LPR), when stomach acid travels up the esophagus and spills into the throat or voice box. However, in most infants, it’s a normal occurrence caused by the immaturity of both the upper and lower esophageal valves, the shorter distance from the stomach to the throat, and the greater amount of time infants spend lying on their backs.
But repeated exposure to acidic stomach contents may cause long-term airway problems, such as a narrowing of the area below the vocal cords, hoarseness, and possibly eustachian tube dysfunction with ear or sinus infections and hearing loss. Infants who have breathing-related symptoms or feeding problems should be seen by an ENT (ear, nose, and throat) specialist, or otolaryngologist.
What Are the Treatment Options?
Treatment of reflux in infants is intended to lessen symptoms, not to relieve the underlying problem, as this will often correct itself over time. Lifestyle changes are often recommended, such as smaller and more frequent feedings, burping more throughout the feeding, avoiding tight diapers and waistbands, and keeping the baby upright after feeding.
You can also help older children make certain lifestyle changes. Pay attention to what they eat, avoiding chocolate, carbonated drinks, caffeine, tomato products, peppermint, and other acidic foods like citrus juices. Fried foods and spicy foods can aggravate GERD symptoms. Have your child eat smaller, more frequent meals instead of large amounts of food at one sitting. Avoid eating right before they go to bed or lie down; let two or three hours pass.
Taking a walk or a warm bath after eating can help your child, as well as losing excess weight or dressing in loose-fitting clothing. You can also try raising the head of your child’s bed about 30 degrees.
Most medications prescribed to treat GERD break down or lessen intestinal gas, decrease or neutralize stomach acid, or improve intestinal coordination. A trial of medications including H2 blockers or proton pump inhibitors may be advised by your child’s primary care physician, but it’s rare for children with GERD to require surgical intervention.
What Questions Should I Ask My Doctor?
- What’s the difference between GERD, LPR, and normal pediatric regurgitation?
- What long-term damage might be done to my child’s development?
- Do you recommend medication or other more intensive forms of treatment?