Hyposmia and Anosmia
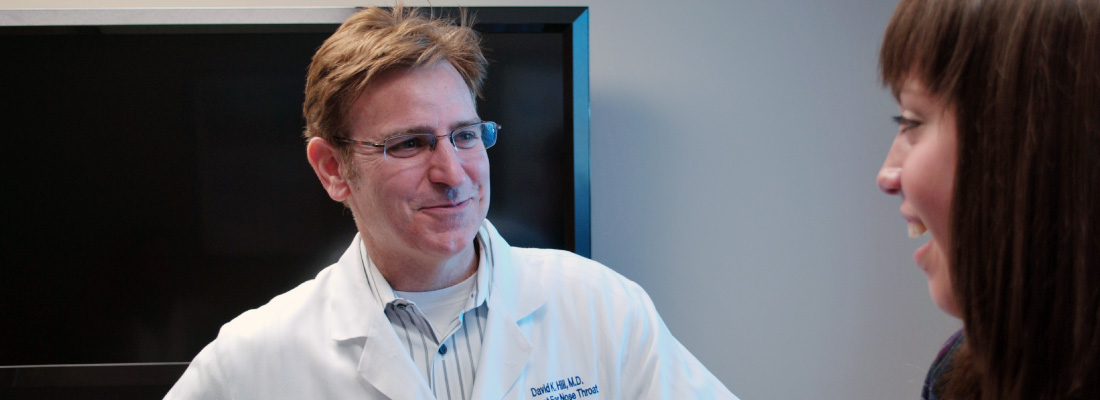
Hyposmia is a decreased sense of smell, or a decreased ability to detect odors through your nose. Anosmia is the inability to smell anything. These conditions are not very common. Smell is one of our most basic, important senses, and has meaning in our lives when it comes to enjoying a new sensation, remembering past experiences, and even detecting potentially dangerous odors such as smoke or spoiled milk. Loss of smell is a health condition that should be evaluated and treated by an ENT (ear, nose, and throat) specialist, or otolaryngologist.
What Are the Symptoms of Hyposmia or Anosmia?
Symptoms of hyposmia or anosmia may be noticed gradually or suddenly, and include:
- Decreased or absent sense of smell
- Decreased sense of taste (flavor is the combination of taste and smell)
- Nasal blockage or congestion
- Nasal inflammation
- Respiratory infection
Losing the ability to smell can often be accompanied by symptoms of chronic sinusitis, which may include frequent infections, facial pressure and pain, nasal obstruction, and drainage. Decreased sense of smell should not be painful or uncomfortable. Since tasting food and beverages is strongly related to the sense of smell, hyposmia or anosmia may also lead to a decreased desire to eat and drink.
What Causes Hyposmia or Anosmia?
The most common cause of acute or sudden smell loss is nasal blockage. Having inflammation in the nose from a cold, allergies, or an upper respiratory tract infection can cause swelling, which blocks smell particles from reaching the top of the nasal cavity where the smell, or olfactory, nerve is located. It is normal to have decreased or loss of smell during an active cold or sinus infection. However, it is less common to have decreased sense of smell when you’re not feeling ill.
Experiencing hyposmia or anosmia over a long period of time may indicate chronic sinus infection with or without nasal polyps. It may be due to an obstruction in the nose, such as a deviated septum, tissue swelling or, rarely, tumors of the nasal cavity. Nasal trauma can cause a loss of smell, either from a new blockage or from damage to the olfactory nerve. Many cases also occur after a viral infection and can be permanent.
Lastly, people often experience a decrease in their sense of smell as a part of normal aging. This is gradual, usually starting after age 65, but it can be sped up by cigarette smoking or chronic nasal inflammation. If you have decreased sense of smell along with memory loss or difficulty walking, tremors, and speech issues, you should tell your primary care provider about these symptoms right away.
What Are the Treatment Options?
Treatment for hyposmia or anosmia starts with figuring out the cause, so seeing an ENT specialist about these conditions is very important, starting with a thorough medical history and nasal exam. This may include a CT scan or MRI of the nose and sinuses. Specialized smell tests can help determine how much loss of smell you may have experienced.
After looking for the cause, your ENT specialist may decide to treat a nasal inflammation or obstruction. This may involve topical and/or oral medications to reduce inflammation, antibiotics, or surgery inside the nose.
Treatment for permanent loss of smell includes environmental safety recommendations and proper chemical detectors (gas and carbon monoxide) in the home. It also may include nasal rinses, smell retraining therapy, and certain supplements that may be helpful.
What Questions Should I Ask My Doctor?
- Why did my sense of smell change?
- What lab or radiology tests do you recommend?
- What medications can I take to try to improve or recover my sense of smell?
- Could I have chronic sinusitis?
- Is my hyposmia or anosmia related to other possible conditions?
Human Papillomavirus (HPV)
HPV, or human papillomavirus, is a sexually transmitted virus. It is not transmitted through casual contact. Many different subtypes of the virus exist, and it usually affects the throat or the reproductive tract. HPV can cause cancer, but not all HPV infections lead to cancer. Most people contract HPV but then clear the virus from their body.
In some people, however, HPV remains in the body causing genetic changes in tissue that can lead to cancer years later. The most commonly affected area by HPV-related cancer is the oropharynx, an area in the throat made up of the tonsils and the base of tongue. Oropharyngeal cancer can also occur unrelated to HPV, usually from smoking and drinking alcohol. HPV-related oropharyngeal cancer carries a better prognosis.
What Are the Symptoms of HPV-related Cancer?
Signs and symptoms of HPV-related oropharyngeal cancer include:
- Lump or swelling in the neck
- Difficulty speaking
- Difficulty or pain when swallowing
- Noticeable sore in the back of the throat
- Earache
- Coughing or spitting up blood
- Weight loss
These symptoms are particularly concerning if they do not go away after a week or two. Early detection significantly improves the chances of a cure.
What Causes HPV-related Cancer?
In a small percentage of people, HPV is contracted through oral-genital contact and develops into oropharyngeal cancer. Infection usually occurs many years before symptoms appear. The risk of HPV-related oropharyngeal cancer can be significantly decreased with currently available vaccines. HPV and/or smoking and tobacco use can increase the risk of oropharyngeal cancer. Smoking or tobacco use with HPV-related oropharyngeal cancer decreases the chance of survival.
What Are the Treatment Options?
HPV-related oropharyngeal cancer can be treated with different types of therapy. Treatment options generally depend on how far the disease has progressed, the specific location and extent of disease, the patient’s health, availability of clinical expertise and equipment, and patient or physician preference.
The two main treatments are surgery and radiation therapy. Surgery can be done in different ways. The majority of these tumors can be removed successfully using surgical instruments through the mouth, including robotic and laser systems. Open surgery, known as a neck dissection, is also typically used to reach the lymph nodes in the neck because cancer cells often spread to these neck lymph nodes. Both sides of the neck often need to be treated.
Radiation therapy can be used as an alternative initial treatment, or as an additional treatment following surgery. Radiation therapy typically involves several weeks of treatment. If given as a primary treatment, it’s possible you may also need surgery later.
There are functional considerations as well as short- and long-term complications associated with both surgery and radiation. Chemotherapy can be used to make tumor cells more sensitive to radiation therapy, called a radiosensitizer, for advanced stages of the disease. This is generally only done when surgery or radiation therapy cannot be given or in a palliative setting, and is not considered to be curative therapy when given by itself.
What Questions Should I Ask My Doctor?
- What can I do to decrease my risk of developing an HPV-related cancer?
- How and when did I contract HPV?
- Is there anything I can do to improve my chance of cure/survival?
- What are the benefits/drawbacks of surgery compared to radiation therapy?
- Is transoral robotic/laser surgery available at this institution? Is there any advantage to these techniques for my tumor?
- If I decide to have surgery, what’s the likelihood I can avoid chemotherapy with radiation?
- What are the risks of surgery?
- What are the risks of radiation therapy?
- Does smoking affect my chance of survival?
- Should I change my sexual practices based on this diagnosis?
Geriatric Rhinitis
Rhinitis is an inflammation of the mucous membranes or lining of the nasal cavity. Geriatric rhinitis, or rhinitis in senior patients, is a common but often neglected or overlooked condition because it is not life-threatening.
Patients with geriatric rhinitis may have nasal obstruction or congestion, runny nose or post-nasal drip, itchy nose, sneezing, and/or nasal dryness or crusting. There are three main types of rhinitis: allergic, non-allergic, and atrophic.
What Are the Symptoms of Geriatric Rhinitis?
For the most part, rhinitis symptoms, diagnosis, and treatment are the same for the elderly as other adult age groups. However, there are special considerations for senior patients, and symptoms of geriatric rhinitis may include:
- Constant feeling of nasal drainage
- Chronic or uncontrolled need to clear the throat of mucus
- Sense of nasal obstruction, most often while lying down
- Nasal crusting, especially during winter and in patients taking diuretics
- Vague facial pressure
- Decreased sense of smell and taste
What Causes Geriatric Rhinitis?
The allergic form of rhinitis is caused by a reaction to various allergens. Elderly patients with symptoms such as repeated sneezing, watery eyes, nasal obstruction with a clear, watery runny nose, and soft, pale turbinates (finger-like structures in the nose that heat and moisten the air you breathe) may have allergic rhinitis. The most common triggers include pollen, mold, dust mites, pet dander, and cockroaches. Allergic reaction to these triggers is diagnosed either by skin prick or blood testing.
Like the allergic form of rhinitis, patients with non-allergic rhinitis may experience nasal congestion, runny nose, and post-nasal drainage. However, these symptoms differ because they do not have an allergic (IgE) component. Non-allergic rhinitis is diagnosed based on the patient’s medical history and the exclusion of other causes. Symptoms can be triggered by changes in temperature, humidity, and exposure to irritating chemicals, smells, or certain medications.
Some older patients are unusually sensitive to environmental, seasonal, and/or physical irritants that don’t bother most people. This is a condition called vasomotor rhinitis, which refers to an overstimulation of the blood vessels (“vaso”) in the nose causing periodic episodes of sneezing, watery drainage, and/or congestion.
Finally, the atrophic form of rhinitis is more common in older adults. A reduction of blood flow to the mucosal lining of the nasal cavity can cause the tissues of the nose to shrink and dry out, causing nasal congestion. This form of rhinitis is associated with nasal dryness, congestion, crusting, and a foul odor if there is an infection.
What Are the Treatment Options?
Treatment for geriatric rhinitis mainly involves medical options. In certain instances, however, surgery may be advised. Treatment for geriatric patients is based not only on the type of rhinitis, but also on the individual patient’s health, medical history, slower metabolism, and increased potential for side effects. Options may include:
Medications—Eighty to 85 percent of elderly patients have chronic diseases and take multiple prescriptions, including over-the-counter medications, to help manage their conditions. Medications to treat geriatric rhinitis, such as intranasal corticosteroids, antihistamines, anticholinergic sprays, and immunotherapy, can place patients at a risk for adverse drug interactions, and should be discussed with a primary care physician or an ENT (ear, nose, throat) specialist, or otolaryngologist.
Surgery—An ENT specialist can determine if surgery of the turbinates is an option. Patients with structural abnormalities, such as a deviated septum or nasal valve collapse causing severe nasal problems, should be referred to an ENT specialist for evaluation.
What Questions Should I Ask My Doctor?
- Do I have rhinitis or sinusitis? What’s the difference?
- How can I improve my condition?
- Will medications to treat geriatric rhinitis interfere with my current medications?
- Do you recommend surgery for my condition?
- Do I need to see an ENT specialist or allergist?