Vestibular Schwannoma (Acoustic Neuroma)
Vestibular schwannoma is a benign (non-cancerous) tumor that grows on the eighth cranial nerve, which is responsible for hearing and balance.
The tumors are rare, accounting for only five to seven percent of all brain tumors. However, for the part of the brain where they are located, called the cerebellopontine angle, it is the most common tumor type.
The annual incidence of being diagnosed with a vestibular schwannoma is one per 100,000 people, with approximately 3,000 newly diagnosed tumors each year in the United States. This number may be rising as our ability to detect smaller tumors has improved. The tumor grows on the eighth cranial nerve, which travels from the inner ear to the brainstem to communicate hearing and balance information to the brain. The nerve has three distinct parts that connect to the inner ear: the superior and inferior vestibular (balance) nerves and the cochlear (hearing) nerve, which come together at the brainstem.
Vestibular schwannomas are also referred to as acoustic neuromas. It was once believed that the tumor originated on the cochlear portion of the eighth cranial nerve because hearing loss is often the first symptom. We now know that the tumor most often arises from one of the vestibular portions of the eighth cranial nerve, therefore the more accurate name is vestibular schwannoma. Both names are still commonly used and refer to the same tumor.
Vestibular schwannomas come in different sizes and cause a variety of problems. This tumor does not spread (metastasize) nor does it invade the brain, but if large enough, it can push on and squeeze the brain.
What Are the Symptoms of a Vestibular Schwannoma?
The symptoms of a vestibular schwannoma may include:
- Sudden or gradual hearing loss (sensorineural hearing loss)
- Ringing, roaring, buzzing, or hissing in the ears or head, known as tinnitus
- Ear fullness
- Vertigo, or feeling like you are spinning when you are still
- Imbalance, or unsteadiness
- Headache
- Facial weakness
- Facial numbness
What Causes a Vestibular Schwannoma?
The exact cause of most vestibular schwannomas is unknown. Ninety-five percent of tumors occur spontaneously and are found on one side (unilateral) only. A small subset of vestibular schwannomas is associated with a genetic condition called Neurofibromatosis Type 2 (NF2). NF2 is rare and results in bilateral vestibular schwannomas. Regardless of the cause, the tumor originates from Schwann cells, which insulate nerves allowing them to transmit their neural signal quickly. When a tumor develops, the Schwann cells grow too quickly and can damage the nerve. In general, vestibular schwannomas grow slowly with an average growth rate of one to two millimeters per year. However, some tumors do not grow for several years and others grow rapidly.
Researchers continue to look for potential causes of vestibular schwannomas. High-dose therapeutic radiation to the head may increase the risk. Overall, there is no clear evidence that environmental factors, such as cell phones, cause these tumors. The rising incidence of vestibular schwannomas likely relates to improvements in magnetic resonance imaging (MRI) and increased screening for concerning symptoms.
What Are the Treatment Options?
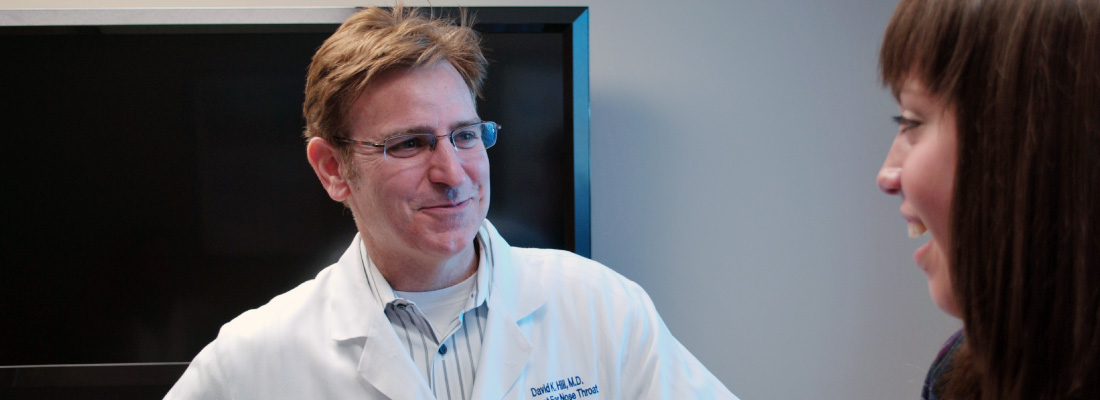
Management of vestibular schwannomas centers around three different options: observation with repeated imaging, radiation, and surgery. The decision is complex and must account for tumor size, hearing status, symptoms, patient health, patient preference, and physician preference. Weighing these factors requires a thorough discussion with your ENT (ear, nose, and throat) specialist, or otolaryngologist, and often referral to additional specialists in neurotology, neurosurgery, and/or radiation-oncology.
Tumors can be classified as small, medium, or large. In general, small tumors are less than 1.5 cm, medium tumors are between 1.5 – 2.5 cm, and large tumors are greater than 2.5 cm. As tumors grow, they tend to cause more problems including hearing loss and compression on the brainstem.
Observation—The “wait and scan” approach may be an option for small tumors or patients for whom treatment carries increased risk. Repeat imaging can help determine the tumor’s growth rate and whether symptoms are changing over time, both of which may influence eventual treatment decisions. In some patients, the tumor may grow at such a slow rate that treatment within their life expectancy is unlikely. With this option, continuing to monitor the tumor with MRIs is critical.
Radiation—Stereotactic radiosurgery (SRS) can be delivered in a single dose or the radiation may be divided into three to five treatment sessions. Radiation is often reserved for growing small- to medium-sized tumors, but other factors should be discussed with your treating physician(s). Different technologies can deliver SRS, such as Gamma Knife®, CyberKnife®, and Triology®. Research has not shown that one radiation technology is better than another. So far, proton beam technology has not been recommended for vestibular schwannoma treatment. In general, the goal of radiation is to stop tumor growth. For some patients, after radiation the tumor may enlarge or swell before it stabilizes or shrinks. Also, long-term hearing often gets worse after radiation. With this option, continuing to monitor the tumor with MRIs is critical.
Surgery—The goal of microsurgery is to remove the tumor while preserving the function of nearby nerves and the brainstem. This option may be selected for a variety of reasons, including large, symptomatic tumors or small tumors with a chance of hearing preservation. There are three primary approaches—behind (retrosigmoid/suboccipital), above (middle cranial fossa), or through (translabyrinthine) the ear—all of which require opening the skull to reach the tumor. The specific approach depends on tumor size, hearing function, and surgeon preference. After surgery, patients can expect a three- to five-day hospital stay. Further details about hospitalization and the risks of surgery should be discussed with the surgeon.
If removing the tumor jeopardizes facial function or brainstem health, a portion of the tumor may be left behind. If the portion of tumor left behind is very small, it can be monitored and sometimes does not grow. If it does grow, radiation or revision surgery may be recommended. If a larger portion of the tumor is left behind, there is an increased likelihood of needing additional treatment.
What Questions Should I Ask My Doctor?
General Questions
- How big is my tumor? Is it growing?
- How is my tumor affecting my hearing?
- What options do I have for treating my hearing loss?
- Are my family members at risk for also having a vestibular schwannoma?
- What kind of specialists might be needed to help manage my tumor and symptoms?
Observation Questions
- What are the risks and benefits of observation (“wait and scan”)?
- How frequently do I need repeat MRIs?
- How frequently do I need hearing tests?
- What will our plan be if the tumor grows?
- What should I do if I experience new symptoms?
Radiation Questions
- What are the risks and benefits of radiation?
- What type of radiation would you use?
- How frequently do I need repeat MRIs?
- How frequently do I need hearing tests?
- In my tumor, do you think radiation will stop its growth?
- What is the plan if the tumor grows despite radiation?
Surgery Questions
- What are the risks and benefits of surgery?
- What type of surgical approach would you recommend?
- How frequently do I need repeat MRIs?
- How frequently do I need hearing tests?
- Can you describe the process for surgical treatment including hospitalization and recovery?
- What is the plan if some tumor is left behind after surgery?
Labyrinthitis
Labyrinthitis is a disorder associated with inflammation of the inner ear. The labyrinth is a fluid-filled compartment that consists of the cochlea and the vestibular organs.
The cochlea is the hearing organ and the vestibular organs are responsible for balance and spatial orientation.
Labyrinthitis has several potential causes, and patients of any age and gender may be affected. Patients with labyrinthitis can experience hearing loss in the affected ear, imbalance, dizziness, and nausea. When the balance organ’s input to the brain is suddenly changed, patients experience vertigo, feeling like you are spinning or moving when you are still. Severe symptoms may limit activities of daily living, the ability to work, and restrict recreational activities.
Labyrinthitis is a self-limiting illness that usually gets better in several weeks. Symptom can begin suddenly and gradually worsen over the course of hours to days before improvement is noticed. Failure to seek treatment may put patients at higher risk for permanent hearing loss and imbalance. Although uncommon, it is possible to have some permanent hearing loss despite treatment. While most patients with imbalance and mild dizziness with head movement recover, sometimes it may take months to years to fully recover. Patients with substantial balance issues may benefit from physical therapy, specifically vestibular physical therapy.
What are the Symptoms of Labyrinthitis?
The symptoms of labyrinthitis can include:
- Hearing loss, often in high frequency pitch range
- Decreased ability to understand speech
- Tinnitus, or ringing or buzzing sensation in the ear
- Imbalance and unsteadiness, falling or swaying to one side while walking
- Vertigo, or feeling like you are spinning when you are still
- Involuntary twitching or jerking of the eyeball, called nystagmus
- Nausea and vomiting
What Causes Labyrinthitis?
Viral infection—Viral infections of the inner ear or activation of a virus that is normally inactive and stays within nerve endings are thought to be the most common cause of labyrinthitis. The specific virus that causes this is usually unknown in most cases. A unique type of labyrinthitis may be caused by reactivation of the varicella-zoster virus, called Ramsay Hunt syndrome, or herpes zoster oticus. This is like shingles of the ear and can occur with labyrinthitis in addition to ear pain, facial weakness, and blisters around the ear, ear canal, and eardrum.
Bacterial infection—A bacterial infection of the middle ear (the space behind the ear drum) can spread to the inner ear and cause bacterial labyrinthitis. Children with inner ear deformities are at a higher risk for bacterial labyrinthitis either from a middle ear infection or from the spread of bacterial meningitis to the inner ear. Severe bacterial labyrinthitis can occur with ear pain, ear infection, drainage of pus from the ear, fevers, or chills. Patients may require hospitalization. This type of infection has a higher risk for permanent hearing loss and may also lead to labyrinthitis ossificans, where there is bone formation in the inner ear after the infection.
Autoimmune—Autoimmune labyrinthitis is a rare cause of labyrinthitis and may come and go. It is often associated with other autoimmune disorders such as systemic lupus erythematosus, inflammatory bowel disease, rheumatoid arthritis, or other autoimmune disorders.
Trauma and surgery—Inner ear trauma puts patients at risk for developing labyrinthitis. Fractures involving the inner ear, concussion of the head and inner ear, or bleeding in the inner ear can cause labyrinthitis.
A tumor of the nerves supplying the inner ear, such as a schwannoma (acoustic neuroma), may also involve hearing loss, vertigo, or labyrinthitis. Your ENT (ear, nose, and throat) specialist, or otolaryngologist, may order an MRI to rule out this condition.
Other potential risk factors include allergies, stress, alcohol and tobacco consumption, and certain medications.
What Are the Treatment Options?
Treating most cases of labyrinthitis includes observation, bed rest, and hydration. Steroids, such as prednisone, are typically prescribed to minimize inner ear inflammation. In some cases, steroids may be injected through the eardrum into the middle ear space. Antivirals may also be prescribed. Severe nausea and vomiting may be treated with anti-nausea medications. Vertigo may be treated with antihistamines or sedatives, such as benzodiazepines, although long-term use will impair the recovery of balance function.
The treatment of bacterial labyrinthitis is to control the primary infection, which is usually a middle ear infection. This may require antibiotics, placement of an ear tube, or more advanced ear surgery. Treatment for autoimmune labyrinthitis addresses the underlying autoimmune condition with steroids or other immune modulating medications usually directed by the rheumatologist.
A multidisciplinary team involving your ENT specialist, audiologist, and vestibular therapist is important to evaluate your hearing, minimize the potential long-term effects of labyrinthitis, and discuss options for possibly restoring your hearing. For severe hearing loss, the patient may be a candidate for a bone-conduction hearing aid or a cochlear implant. When the balance organs are damaged, the brain needs time to adjust to improve balance function again. Vestibular therapy and balance exercises help many patients regain their balance.
Although labyrinthitis is not life-threatening, vertigo may rarely be a sign of a more serious disorder such as a stroke or brain tumor. Patients with sudden, persistent vertigo or additional worsening symptoms such as double vision, slurred speech, facial droop, limb weakness, or numbness should seek immediate medical attention.
What Questions Should I Ask My Doctor?
- What are my treatment options?
- When should I get a repeat hearing evaluation?
- What tests should I have performed?
- Do I need an MRI?
- What are the options for hearing restoration?
- Should I seek vestibular therapy?
Autoimmune Inner Ear Disease
Autoimmune inner ear disease (AIED) is an inflammatory condition caused by an uncontrolled immune system response that attacks the inner ear causing progressive sensorineural hearing loss (SNHL) that usually starts in one ear and then affects the other ear.
The body thinks a part of the inner ear should not be there and makes antibodies and immune, also called antigen-antibody, complexes that attack the inner ear. This causes blood vessel inflammation, inner ear tissue damage, and hearing loss. Antigens are the molecules that cause an immune response and antibodies are proteins that protect the body against these antigens.
AIED is rare and diagnosed only when all other causes have been ruled out. The estimated prevalence of AIED is about 15 out of 100,000 people. AIED is felt to be responsible for less than one percent of all SNHL cases, realizing many AIED cases might not be diagnosed due to lack of specific tests.
AIED is considered “primary” when the inner ear is the only organ affected. However, in 15 to 30 percent of cases, AIED is “secondary” when it occurs as part of a larger autoimmune disorder that affects the whole body, such as rheumatoid arthritis, lupus, scleroderma, ulcerative colitis, or Sjogren’s syndrome. AIED is more common among middle-aged women.
Diagnosing AIED is challenging because there is no definite blood or imaging criteria to measure. Timing the progression of hearing loss over weeks to months is an important diagnostic clue for AIED. If AIED is suspected, early corticosteroid and immunosuppressive treatment may prevent irreversible hearing loss. A multidisciplinary team approach between an ENT (ear, nose, and throat) specialist, or otolaryngologist, an audiologist, and a rheumatologist is recommended to manage the condition.
What Are the Symptoms of AIED?
Common symptoms of AIED can include:
- Progressive SNHL in both ears that occurs over weeks to months that is not always the same in both ears
- Fluctuating hearing
- Dizziness or imbalance (approximately 50 percent of AIED cases)
- Ringing in the ears, or tinnitus
- Ear fullness (approximately 25 to 50 percent of AIED cases)
- Conductive hearing loss may be present due to Eustachian tube obstruction from inflamed middle ear lining and/or if AIED is because of systemic autoimmune diseases
- Symptoms of systemic autoimmune diseases, such as fatigue, achy muscles, swelling and redness, low-grade fever, and more
What Causes AIED?
The causes of AIED can include:
- The body’s uncontrolled immune system attacks the inner ear protein, forming immune complexes and antibodies and causing progressive hearing loss in both ears.
- Cochlin is a protein located in the inner ear that is attacked by the immune system.
- Endolymphatic sac, a structure of the inner ear, can become dilated as the immune response of the inner ear.
What Are the Treatment Options?
If you are having hearing loss that is getting worse in both ears over weeks to months, you should see an ENT specialist who can make a diagnosis after reviewing your hearing tests and imaging scans. If your doctor suspects that you may have AIED, you may respond well to medical therapy—steroid and immunosuppressive medication—if started early.
Corticosteroid is the main treatment to suppress the immune response to reduce inner ear swelling and inflammation. Early detection of AIED and prompt steroid treatment may help reverse your SNHL. If you cannot tolerate steroid treatment, there are alternative medications, such as cyclophosphamide, methotrexate, azathiorprine, and rituximab.
Your doctor may also evaluate you for a hearing aid or other assistive listening devices. If hearing loss is substantial, your doctor may recommend a hearing device called a cochlear implant. Speak with your doctor about other specific treatment options.
What Questions Should I Ask My Doctor?
- Do I have a systemic autoimmune disorder?
- What tests should I have performed to evaluate my hearing loss?
- Do I need to get an MRI to rule out other inner ear disorders?
- What are my treatment options for AIED?
- What medications are available to me?
- What other healthcare professionals should I see for AIED?
Turbinate Hypertrophy
Turbinate hypertrophy refers to an excessive growth or enlargement of the turbinates, which are bony structures located inside the nose. They are covered with a special skin called mucosa, and they help filter, warm, and humidify the air as you breathe. The mucosa naturally swells during the normal nasal cycle and when you lie down. They also swell in response to allergens and other stimuli.
The nasal cavity usually contains three sets of turbinates on each side of the nose: the superior turbinates, the middle turbinates, and the inferior turbinates. Most of the airflow in the nose passes between the middle and inferior turbinates. If these turbinates become enlarged, breathing can become more difficult.
What Are the Symptoms of Turbinate Hypertrophy?
The most common symptoms of turbinate hypertrophy include:
- Difficulty breathing
- Congestion in alternating sides of the nose
- Nasal stuffiness
- Nasal blockage
- Nasal congestion while lying down
- Noisy breathing or breathing through the mouth during sleep
- Increased nasal drainage
What Causes Turbinate Hypertrophy?
Turbinate hypertrophy is typically caused when the lining of the skin covering the turbinate bone becomes enlarged and swollen. This can be an acute (one time) or chronic (ongoing) problem, and can be caused by many conditions including:
- Upper respiratory infection, or the common cold
- Acute sinus infection
- Allergic rhinitis
- Non-allergic rhinitis
- Chronic rhinosinusitis
- Medications
- Hormonal changes
Other related factors or conditions that can cause nasal blockage include a deviated septum, nasal valve collapse, and external nasal deformity, or other kind of sinus disease.
What Are the Treatment Options?
Treating turbinate hypertrophy depends on the specific cause. First, discuss your symptoms with your primary care physician or an ENT (ear, nose, and throat) specialist, or otolaryngologist. They will examine your nose and may recommend additional tests, such as allergy testing or X-rays, depending on your specific diagnosis.
Medical therapy—Medications are often suggested to help reduce symptoms. Depending on the specific cause of the turbinate hypertrophy, possible medications include:
- Nasal saline sprays or rinses
- Nasal antihistamine sprays
- Nasal steroid sprays
- Allergy immunotherapy
For an acute case of turbinate hypertrophy, nasal decongestant sprays (such as Oxymetazoline) should only be used for a very brief period. This is not an appropriate treatment for chronic turbinate hypertrophy. Using nasal decongestant sprays for longer than three days can result in additional swelling in the nasal cavity, worsening symptoms, and addiction with prolonged use.
Surgery—If medications do not help improve your symptoms, your ENT specialist may offer a surgical procedure to decrease the size of the turbinates. This procedure is usually performed through the nostrils and does not result in bruising or an outward sign of surgery.
The goal of surgery is to decrease the size of the turbinate to improve airflow through the nose while preserving the function of the turbinate. There are many different types of surgical procedures to reduce the size of the turbinates, and will depend on your specific diagnosis, the severity of the turbinate hypertrophy, and your ENT specialist’s recommendation. Many of these procedures can be done in the office using specialized devices that can reduce the size of the turbinates while leaving the special skin (mucosa) intact.
Surgery can usually be performed under local or general anesthesia as an outpatient procedure, and may be combined with other procedures to reduce nasal obstruction. The most common associated procedure is called a septoplasty to address a deviated septum.
Complications from turbinate surgery are rare but can include:
- Anesthesia complications
- Pain
- Swelling
- Bleeding
- Infection
- Dryness and crusting inside the nasal cavity
- Regrowth of the turbinate swelling and recurrent nasal congestion
Empty nose syndrome (ENS) is an unusual condition that can occur after turbinate surgery, and is usually associated with significant resection of the turbinates. In this condition, the nose continues to feel congested and obstructed despite the nasal passage being opened after surgery. This is an extremely rare condition and not completely well understood; if you have concerns about having or developing ENS, discuss this with your ENT specialist.
What Questions Should I Ask My Doctor?
- What is the most likely cause of my turbinate hypertrophy?
- Which medications are best suited to treat my turbinate hypertrophy?
- Are there any other conditions that could be contributing to my nasal congestion?
- Should I have any other evaluations? Allergy testing? Consultations with other specialists?