Temporo-Mandibular Joint (TMJ) Pain
“TMJ” pain is a common occurrence for many people, and it refers to pain or discomfort in the Temporo-Mandibular Joint (TMJ). This is the hinge that connects your temporal bone (the bone that forms the side of the skull) and your mandible (the lower jaw) in front of your ear, making it possible for you to open and close your mouth. Think of your jaw as a lever; the TMJ is vital because it supports that lever. When you bite down, you put force on the object between your teeth and on the joint. Even though it is only a small disc of cartilage, the TMJ separates the bones so you can talk, swallow, chew, kiss, etc. When it is damaged, it can cause a significant amount of pain.
What Are the Symptoms of TMJ Pain?
Common symptoms of TMJ pain may include:
- Ear pain
- Sore jaw muscles
- Temple or cheek pain
- Jaw popping/clicking
- Locking of the jaw
- Difficulty in opening the mouth fully
- Frequent head and/or neck aches
- Ringing in the ears (also called tinnitus)
Your pain may be sharp and searing, occurring each time you swallow, yawn, talk, or chew, or it may be dull and constant. It hurts over the joint, immediately in front of the ear, but pain can also radiate elsewhere. It often causes spasms in the adjacent muscles attached to the bones of the skull, face, and jaws. Pain can also be felt at the side of the head (the temple), the cheek, the lower jaw, and the teeth.
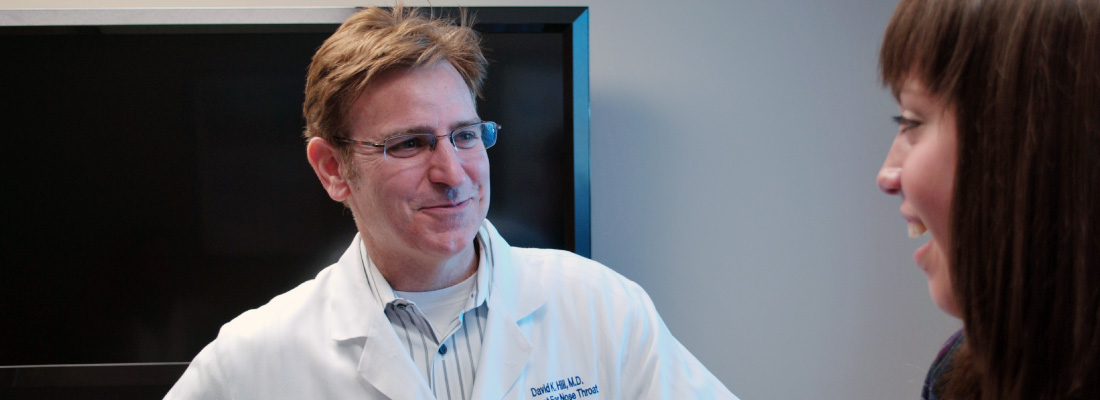
A common focus of pain is in the ear. Many patients see an ENT (ear, nose, and throat) specialist, or otolaryngologist, convinced that their pain is from an ear infection. When the earache is not associated with a hearing loss and the eardrum looks normal, the ENT specialist will consider the possibility that the pain comes from TMJ.
What Causes TMJ Pain?
In most patients, TMJ pain is a result of movement or displacement of the cartilage disc that causes pressure and stretches certain sensory nerves. Popping or clicking noises occur when the disk snaps into place when the jaw moves. In addition, the chewing muscles may spasm or not function efficiently, causing pain and tenderness. These actions or situations can also damage the TMJ:
- Major and minor trauma to the jaw
- Teeth grinding
- Excessive gum chewing
- Stress and other psychological factors
- Improper bite or improperly positioned jaws
- Arthritis
What Are the Treatment Options?
When you see your primary care physician or an ENT specialist about your TMJ pain, they will start with a detailed medical history and physical, looking to see how your teeth come together when you bite down. They will also examine how the joints and muscles around your jaw function. Depending on your case, your doctor may recommend trying simple, self-remedies to help relieve TMJ pain such as:
- Resting your muscles and joints by eating soft foods
- Not chewing gum
- Not clenching or tensing your jaw
- Relaxing your muscles with moist heat
In cases of joint injury, your doctor may recommend applying an ice pack soon after the injury to reduce swelling. Relaxation techniques and stress reduction, non-steroidal anti-inflammatory drugs, muscle relaxants, or other medications may also offer relief.
Other treatments for advanced cases may include an occlusal splint, or mouth guard, to prevent wear and tear on the joint, improving the alignment of the upper and lower teeth, and surgery. Your ENT specialist may also suggest additional consultation with your dentist and oral surgeon to help manage your TMJ pain.
What Questions Should I Ask My Doctor?
- The area around my jaw really hurts. My dentist said that nothing is wrong with my teeth and suggested that I might have an ear infection. What should I do next?
- Should I see a specialist?
- What can I do to prevent or treat TMJ pain without having to go back to the doctor?
- Is TMJ pain hereditary?
- How many people get TMJ pain?
Swimmer’s Ear (Otitis Externa)
Swimmer’s ear (also called acute otitis externa) is a painful condition that affects the outer ear and ear canal that is caused by infection, inflammation, or irritation. These symptoms often occur after water gets trapped in your ear, especially if the water has bacteria or fungal organisms in it. Because this condition commonly affects swimmers, it is known as swimmer’s ear.
Swimmer’s ear often affects children and teenagers, but can also affect those with eczema (a condition that causes the skin to itch), those with highly sensitive or allergic skin reactions, excess earwax, and who wear hearing aids or earbuds. Your primary care provider or ENT (ear, nose, and throat) specialist, or otolaryngologist, will prescribe treatment to reduce your pain and to treat the infection.
What Are the Symptoms of Swimmer’s Ear?
Signs and symptoms of swimmer’s ear may include:
- Itching inside the ear (common)
- Pain inside the ear that gets worse when you tug on the outer ear (common)
- Sensation that the ear is blocked or full
- Drainage from the ear
- Fever
- Decreased hearing
- Intense pain that may spread to the neck, face, or side of the head
- Swollen lymph nodes around the ear or in the upper neck
- Redness or swelling of the skin around the ear
If left untreated, a certain amount of hearing loss may occur. When the infection clears up, hearing usually returns to normal. Recurring ear infections (chronic otitis externa) are also possible. Without treatment, infections can continue to occur or persist.
Bone and cartilage damage (malignant otitis externa) are also possible due to untreated swimmer’s ear. If left untreated, ear infections can spread to the base of your skull, brain, or cranial nerves. Diabetics, older adults, and those with conditions that weaken the immune system are at higher risk for such dangerous complications.
To evaluate you for swimmer’s ear, your doctor will look for redness and swelling in your ear canal, and ask if you are experiencing any pain. Your doctor may also take a sample of any abnormal fluid or discharge in your ear (ear culture) to test for the presence of bacteria or fungus if you have recurrent or severe infections.
What Causes Swimmer’s Ear?
A common source of the infection is increased moisture trapped in the ear canal from baths, showers, swimming, or moist environments. When water is trapped in the ear canal, bacteria that normally inhabit the skin and ear canal multiply, causing infection of the ear canal. Swimmer’s ear needs to be treated to reduce pain and eliminate any effect it may have on your hearing, as well as to prevent the spread of infection.
Other factors that may contribute to swimmer’s ear include:
- Contact with excessive bacteria that may be present in hot tubs or polluted water
- Excessive cleaning of the ear canal with cotton swabs or anything else that may cause breaks in the ear canal skin allowing bacteria in
- Contact with certain chemicals such as hair spray or hair dye (avoid this by placing cotton balls in your ears when using these products)
- Damage to the skin of the ear canal following water irrigation to remove wax
- A cut in the skin of the ear canal
- Other skin conditions affecting the ear canal, such as eczema or seborrhea
Finally, what’s often called swimmer’s ear can also caused by ill-fitting hearing aids, or contaminated earbuds, earphones, or other ear devices.
What Are the Treatment Options?
Treatment for the early stages of swimmer’s ear includes careful cleaning of the ear canal and use of eardrops that inhibit bacterial or fungal growth and reduce inflammation. Mildly acidic solutions containing boric or acetic acid are often effective for early infections.
Before using any drops in the ear, it is important to be sure you do not have a perforated eardrum (an eardrum with a hole in it). Check with your ENT specialist if you have ever had a perforated, punctured, or injured eardrum, or if you have had prior ear surgery.
Drops are more easily administered if done by someone other than the patient, and the patient should lie down with the affected ear facing upwards. Prescription drops should be placed in the ear as directed on the label. After drops are administered, the patient should remain lying down for a few minutes, so the drops have time to work.
If you do not have a perforated eardrum or a tube in your eardrum placed by a doctor in the past, you can make your own eardrops using rubbing alcohol or a mixture of half alcohol and half vinegar. These eardrops will evaporate excess water and keep your ears dry.
For more severe infections, your doctor may prescribe antibiotics to be applied directly to the ear. If the ear canal is swollen shut, your doctor may place a sponge or wick in the canal so the antibiotic drops will enter the swollen canal more effectively. Pain medication may also be prescribed. If you have tubes in your eardrum, a non-ototoxic (do not damage your hearing) topical treatment should be used. Topical antibiotics are effective for infection limited to the ear canal. Oral antibiotics may also be prescribed if the infection goes beyond the skin of the ear canal.
Follow-up appointments are very important to monitor your condition, to clean the ear again, and to replace the ear wick as needed. Your ENT specialist has specific equipment and expertise to effectively clean the ear canal and treat swimmer’s ear. With proper treatment, most infections should clear up in seven to 10 days.
How Can Swimmer’s Ear be Prevented?
A dry ear is unlikely to become infected, so it is important to keep the ears free of moisture during swimming or bathing. Prevention tips include:
- Use ear plugs when swimming.
- Use a dry towel or hair dryer (from a distance) to dry your ears.
- Have your ears cleaned periodically by an ENT specialist if you have itchy, flaky or scaly ears, or extensive earwax.
- Do not use cotton swabs to remove ear wax. They may pack ear wax and dirt deeper into the ear canal, remove the layer of earwax that protects your ear, and irritate the thin skin of the ear canal. This creates an ideal environment for infection.
What Questions Should I Ask My Doctor?
- What can I use at home for pain control for my child or me?
- Can my child swim while having swimmer’s ear?
- My child has excess ear wax. Can I use cotton swabs to help remove it?
Sore Throats
Sore throats happen to everyone now and then. When you have a sore throat, this can affect speaking, swallowing, or breathing.
Infections from viruses or bacteria are the main cause of sore throats, but allergies and sinus infections can also contribute. Some sore throats are worse than others. If you have a sore throat that lasts for more than five to ten days, you should see your doctor.
What Are the Symptoms of a Sore Throat?
Whenever a sore throat is severe, lasts longer than the usual five- to ten-day duration of a cold or flu, and is not associated with an avoidable allergy or irritation, you should seek medical attention. The following signs and symptoms should alert you to see your physician:
- Severe and prolonged sore throat
- Difficulty breathing
- Difficulty swallowing
- Difficulty opening the mouth
- Swelling of the face or neck
- Joint pain
- Earache
- Rash
- Fever (over 101°F)
- Blood in saliva or phlegm
- Frequently recurring sore throat
- Lump in neck
- Hoarseness lasting over two weeks
What Causes a Sore Throat?
Infections by contagious viruses or bacteria are the source of most sore throats. Other potential causes include:
Viruses—Sore throats often accompany viral infections, including the flu, colds, measles, chicken pox, croup, or mononucleosis (mono). Mono has the longest duration of symptoms, such as sore throat and extreme fatigue, and can last several weeks. Other symptoms include swollen glands in the neck, armpits, and groin; fever, chills, headache, or sometimes, serious breathing difficulties.
Bacterial infection—Strep throat is an infection caused by Streptococcus bacteria. This infection can also cause scarlet fever, tonsillitis, pneumonia, sinusitis, and ear infections. Symptoms of strep throat often include fever (greater than 101°F), white draining patches on the throat, and swollen or tender lymph glands in the neck. Children may have a headache and stomach pain.
Pertussis, also known as whooping cough, is a highly contagious respiratory disease caused by Bordetella pertussis bacteria. This infection can bring about violent, uncontrollable coughing, making it hard to breathe and causing you to make a “whooping” sound. Whooping cough can affect people of all ages, but can be especially serious, even deadly, for babies less than one-year-old.
Epiglottitis—Epiglottitis is the most dangerous throat infection, because it causes swelling that closes the airway and requires prompt emergency medical attention. Suspect it when swallowing is extremely painful (causing drooling), when speech is muffled, and when breathing becomes difficult. Epiglottitis is often not seen just by looking in the mouth.
Allergies—You may also be allergic to pollens, molds, animal dander, and/or house dust, for examples, which can lead to a sore throat.
Irritation—Dry heat, dehydration, chronic stuffy nose, pollutants, car exhaust, chemical exposure, or straining your voice are examples of irritations that can lead to a sore throat.
Reflux—Reflux occurs when you regurgitate stomach contents up into the throat. You may notice this often in the morning when you first wake up. Reflux that goes into the throat is called laryngopharyngeal reflux (LPR).
Tumors—Tumors of the throat, tongue, and larynx (voice box) can cause a sore throat with pain going up to the ear. Other important symptoms can include hoarseness, difficulty swallowing, noisy breathing, a lump in the neck, unexplained weight loss, and/or spitting up blood in the saliva or phlegm.
What Are the Treatment Options?
A mild sore throat associated with cold or flu symptoms can be made more comfortable with the following remedies:
- Increase your liquid intake.
- Drink warm tea with honey (a favorite home remedy).
- Use a personal steamer or place a humidifier in your bedroom.
- Gargle with warm salt water several times daily: ¼ tsp salt to ½ cup water.
- Take over-the-counter pain relievers such as acetaminophen (Tylenol Sore Throat®, Tempra®) or ibuprofen (Motrin IB®, Advil®).
For a more severe sore throat, your doctor may want to do a throat culture—swabbing the inside of your throat to see if there is a bacterial infection. If it is negative, your physician will base their treatment recommendation on the severity of your symptoms and the appearance of your throat on examination.
If you have a bacterial infection your doctor will likely recommend an antibiotic (such as penicillin or erythromycin) that kills or impairs bacteria. Antibiotics do not cure viral infections, but viruses do lower the patient’s resistance to bacterial infections. When a combined infection like this happens, antibiotics may be recommended.
It is important to take an antibiotic as your physician directs and to finish all doses, even if your symptoms improve, otherwise the infection may not be gone and could return. Some patients will experience returning infections despite antibiotic treatment. If you experience this, it is important to discuss this situation with your physician.
You may also want to review these Sore Throat Prevention Tips.
What Questions Should I Ask My Doctor?
- Is my sore throat the same as strep throat?
- How long before this sore throat goes away?
- How do I know if my sore throat is a serious problem?
- Should I take antibiotics to treat my sore throat?
Snoring, Sleeping Disorders and Sleep Apnea
Nearly half of adults snore, and over 25 percent are habitual snorers. Problem snoring and sleeping disorders are more frequent in males and people who are overweight, and usually worsens with age. Snoring is bothersome to others, but it can also be a sign of a more serious condition known as obstructive sleep apnea (OSA), which is present in three percent of the general population. OSA is characterized by multiple pauses in breathing greater than 10 seconds at a time due to upper airway narrowing or collapse. This lowers the amount of oxygen in the blood, and causes the heart to work harder. Because the snorer does not get a good rest, they may be sleepy during the day, which decreases their performance. Untreated OSA can contribute to high blood pressure, stroke, heart disease, workplace or motor vehicle accidents, and more.
What Are the Symptoms of OSA?
Symptoms associated with OSA can include:
- Loud snoring
- Pauses in breathing during sleep
- Waking up gasping or choking
- Waking up with a dry mouth or sore throat
- Daytime sleepiness or fatigue
- Frequent nighttime urination
- Morning headache
- Irritability, mood changes, depression, difficulty concentrating
- High blood pressure, heart disease, stroke, or other cardiac issues
What Causes OSA?
The noisy sounds of snoring occur when there is a partial obstruction to the flow of air through the passages at the back of the mouth and nose. This area is the collapsible part of the airway where the tongue and upper throat meet the soft palate and uvula. Snoring occurs when these structures strike each other and vibrate during breathing. Apnea occurs when the obstruction of air flow is more severe, leading to reduced, compromised, or completely blocked air flow while trying to breathe.
In children, snoring may be a sign of problems with the tonsils and adenoids. In adults, the site of obstruction may not be as simple to identify. Obstruction in an adult may be due to a combination of factors in different areas, making it more challenging to identify and treat.
What Other Factors Contribute to Snoring and Sleep Apnea?
Poor muscle tone in the tongue and throat—When muscles are too relaxed, the tongue falls backward into the airway, or the throat muscles draw in from the sides into the airway. Alcohol or drugs that cause sleepiness may worsen muscle relaxation and obstruction.
Excessive bulkiness of throat tissue—Children with large tonsils and adenoids often snore. Overweight people may have excess soft tissue in the neck that can lead to airway narrowing. Those with very large tongues are especially susceptible to snoring and OSA. Cysts or tumors are rare causes of airway narrowing.
Long soft palate and/or uvula—A long palate narrows the opening from the nose into the throat. The excessive length of the soft palate and/or uvula acts as a noisy flutter valve during relaxed breathing.
Obstructed nasal airways—A stuffy nose requires extra effort to pull air through it. This creates an exaggerated vacuum in the throat that pulls together the floppy tissues of the throat. Sometimes, snoring only occurs during allergy season or with a cold or sinus infection. Deformities of the nose or nasal septum, such as a deviated septum (a deformity of the wall that separates one nostril from the other) can also cause snoring and OSA.
What Are the Treatment Options?
Heavy snorers—people who snore constantly in any position or who negatively impact a bed partner’s sleep—should seek medical advice to ensure that sleep apnea is not a problem. An ENT (ear, nose, and throat) specialist, or otolaryngologist, will provide a thorough examination of the nose, mouth, throat, palate, and neck, often using a fiberoptic scope. An examination can reveal if the snoring is caused by nasal allergy, infection, nasal obstruction, or enlargement of tonsils and adenoids. A sleep study in a laboratory or at home may be necessary to determine if snoring is due to OSA.
OSA is most often treated with a device that opens the airway with a small amount of positive pressure. This pressure is delivered by an appliance through either the nose and/or mouth that is worn during sleep. This treatment is called continuous positive airway pressure, or CPAP, and it is currently the initial treatment of choice for patients with OSA. The challenge of treating OSA is that obstruction can occur at multiple levels of the airway. CPAP stabilizes pressure at all parts of the upper airway and can be very effective, but some wearers cannot tolerate CPAP and must seek other options.
A custom-fit oral appliance, which repositions the lower jaw forward, may also be considered for certain patients with snoring/OSA. This should be fitted by an ENT specialist, dentist, or oral surgeon with expertise in sleep dentistry. In some patients, significant weight loss can also improve snoring and OSA.
There are numerous surgical treatments for snoring/OSA, including:
- Uvulopalatopharyngoplasty (UPPP) is a plastic surgery of the throat involving tissue repositioning, or removal of excess soft tissue, to open the airway. In addition, the remaining tissue stiffens as it heals, helping to minimize tissue vibration. A tonsillectomy can also help enlarge the airway.
- Thermal ablation procedures reduce tissue bulk in the nasal turbinates (structures on the side wall of the inside of the nose), tongue base, and/or soft palate. These procedures are used for both snoring and OSA, and several treatments may be required.
- The soft palate may be stiffened by inserting stiffening rods into the soft palate, or by injecting an irritating substance that causes stiffness in the injected area near the uvula.
- “Hypoglossal nerve stimulator” technology implants a tongue pacemaker, which stiffens and projects the tongue forward during sleep. Other procedures may be used to surgically target tongue muscles or the boney configuration of the midface.
Read more about surgery for OSA
What Questions Should I Ask My Doctor?
- When should I consider having a sleep study?
- What is the likelihood that sleep apnea can affect my overall health, or shorten my lifetime?
- There are so many treatments available, how do I decide?
- Is sleep apnea a genetic disease?
- What conservative treatments are available?